For decades, Polycystic Ovarian Syndrome (PCOS) has been framed as a reproductive disorder defined by cysts on the ovaries.
But here’s the truth:
👉 Many women with PCOS do not have ovarian cysts.
👉 Many women with ovarian cysts do not have PCOS.
So why are we still using a name that implies cysts are required for diagnosis?
This misunderstanding leads to missed diagnoses, delayed care, and years of unnecessary frustration—especially for women who don’t “look” like a classic PCOS case.
It’s time to update the conversation.
PCOS Is Not Really About Cysts
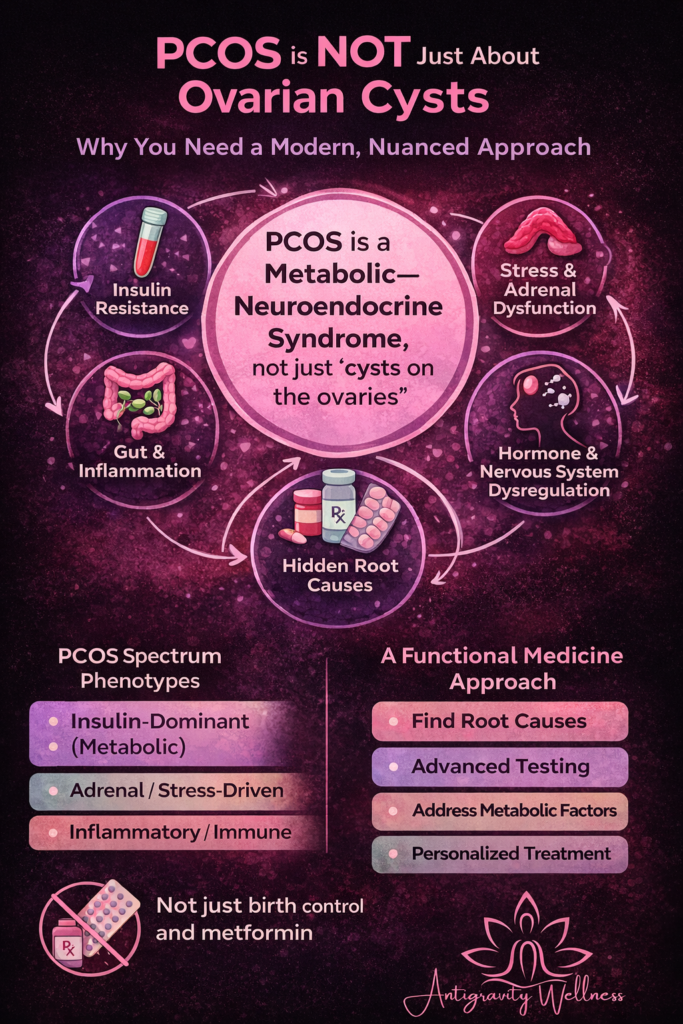
Despite its name, PCOS is best understood as a metabolic–neuroendocrine syndrome, not a structural ovarian disease.
The ovaries are often the visible expression of a deeper problem—but they are rarely the root cause.
PCOS involves dysregulation across:
- Insulin signaling
- Androgen production
- Brain–ovary communication
- Inflammation
- Stress physiology
- Gut and liver metabolism
That’s why PCOS looks different from woman to woman—and why a one-size-fits-all approach fails so often.
How PCOS Is Actually Diagnosed
Most guidelines still use the Rotterdam criteria, which require 2 out of 3 of the following (after excluding other conditions):
- Irregular or absent ovulation
- Clinical or biochemical hyperandrogenism
(acne, hair growth, hair loss, elevated androgens) - Polycystic ovarian morphology on ultrasound
📌 Ultrasound is not required for diagnosis.
📌 A normal ultrasound does not rule out PCOS.
This is where many women get told:
“Your labs are normal.”
“Your ultrasound looks fine.”
“You don’t have PCOS.”
—when in reality, they’re living with clear symptoms.
PCOS Is a Spectrum, Not a Yes/No Diagnosis
Clinically, PCOS behaves more like:
- Insulin resistance
- Autoimmune conditions
- Endometriosis
…than a binary disease.
There are distinct PCOS phenotypes, including:
- Insulin-dominant (metabolic)
- Adrenal/stress-driven
- Inflammatory or immune-mediated
- Post-pill or hypothalamic patterns
- Mixed/genetic susceptibility
Most women have one dominant driver with secondary contributors—which is why identifying their pattern matters so much.
Why Traditional Care Often Misses the Diagnosis
Conventional care typically focuses on:
- Period regulation
- Acne suppression
- Fertility assistance
Often using:
- Birth control
- Spironolactone
- Metformin (sometimes)
While these can be helpful tools, they do not explain why PCOS is happening—and in many cases, symptoms return when medication stops.
Time constraints, insurance models, and limited testing make it difficult to explore:
- Insulin dynamics beyond glucose and A1c
- Adrenal function
- Inflammatory markers
- Nutrient deficiencies
- Gut and liver metabolism
This is where a functional medicine approach shines.
Why Functional Medicine Is Better Suited for PCOS
Functional medicine asks a different question:
“What’s driving this person’s PCOS?”
At Antigravity Wellness, we evaluate:
- Metabolic signaling (not just blood sugar)
- Hormone patterns across the cycle
- Stress and nervous system load
- Inflammatory and immune markers
- Gut health and detoxification capacity
- Lifestyle, sleep, training, and nutrition patterns
Treatment is not just medication—it’s a personalized strategy that may include:
- Nutrition tailored to insulin and inflammation
- Strength training and movement guidance
- Stress and nervous system regulation
- Gut healing protocols
- Targeted supplementation
- Medication when appropriate, not as a default
Case Study #1: Under 35, Missed for Years
“I kept being told I was just gaining weight because I was getting older.”
Sarah, 32, came to Antigravity Wellness frustrated and confused.
Her symptoms:
- Gradual weight gain despite “doing everything right”
- Fatigue
- Acne flares
- Cycles that were mostly regular—until suddenly they weren’t
Her labs with primary care?
“Normal.”
No ultrasound. No further evaluation. No answers.
Within her first 6-week starter package, we identified:
- Early insulin resistance
- Elevated androgens
- A metabolic-dominant PCOS phenotype
“For the first time, someone explained why my body was responding this way.”
With targeted nutrition, strength training, stress support, and metabolic optimization, she began feeling better within weeks—and finally had a clear plan forward.
Case Study #2: PCOS in Perimenopause (Often Overlooked)
“I thought PCOS was something you had when you were young.”
Melissa, 46, came in with:
- Weight gain around the midsection
- Worsening fatigue
- Hair thinning
- Mood changes
- Irregular cycles she attributed to perimenopause
Her ultrasound was “normal.”
She’d been told PCOS didn’t apply anymore.
But functionally, she showed:
- Longstanding insulin resistance
- Androgen imbalance
- Inflammatory signaling amplified by hormonal shifts of perimenopause
“Everything finally made sense when it was explained as a pattern, not a label.”
By addressing metabolism, inflammation, stress, and hormone balance together, she saw improvements in energy, weight stability, and confidence—without chasing symptoms one by one.
PCOS Needs a New Name—and a Better Approach
PCOS is not about cysts.
It’s not just about fertility.
And it’s not solved with a single prescription.
It’s a complex syndrome that deserves individualized care.
At Antigravity Wellness, we work with PCOS patients across life stages to:
- Identify their dominant phenotype
- Address root causes
- Prevent long-term metabolic and cardiovascular complications
- Create sustainable, realistic treatment plans aligned with their goals
If you’re wondering whether our approach is a good fit for you, we invite you to start with our Readiness Questionnaire to explore next steps.
Medical Disclaimer
This article is for educational purposes only and does not constitute medical advice. Diagnosis and treatment decisions should always be made in partnership with a qualified healthcare provider.
References
- Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Hum Reprod. 2004. https://www.scirp.org/reference/referencespapers?referenceid=2828386
- Teede HJ et al. International Evidence-Based Guideline for PCOS. Hum Reprod Update. 2018. https://pubmed.ncbi.nlm.nih.gov/30052961/
- Diamanti-Kandarakis E et al. Insulin resistance in PCOS. Endocr Rev. 2007. https://pubmed.ncbi.nlm.nih.gov/17185787/
- Dumesic DA et al. Scientific Statement on PCOS. Endocr Rev. 2015. https://pubmed.ncbi.nlm.nih.gov/26426951/
- Azziz R et al. PCOS as a metabolic disorder. Nat Rev Endocrinol. 2016. https://pubmed.ncbi.nlm.nih.gov/27510637/