Endometriosis is one of the most underdiagnosed and misunderstood conditions in women’s health.
Despite affecting an estimated 1 in 10 women, many are told for years that:
- “Painful periods are normal”
- “It’s just stress”
- “Your imaging looks fine”
- “Birth control is the only option”
For many women, it takes 7–10 years to receive a diagnosis—often after years of physical pain, emotional distress, and feeling dismissed.
The problem isn’t that endometriosis is rare.
The problem is that we’ve been looking at it too narrowly.
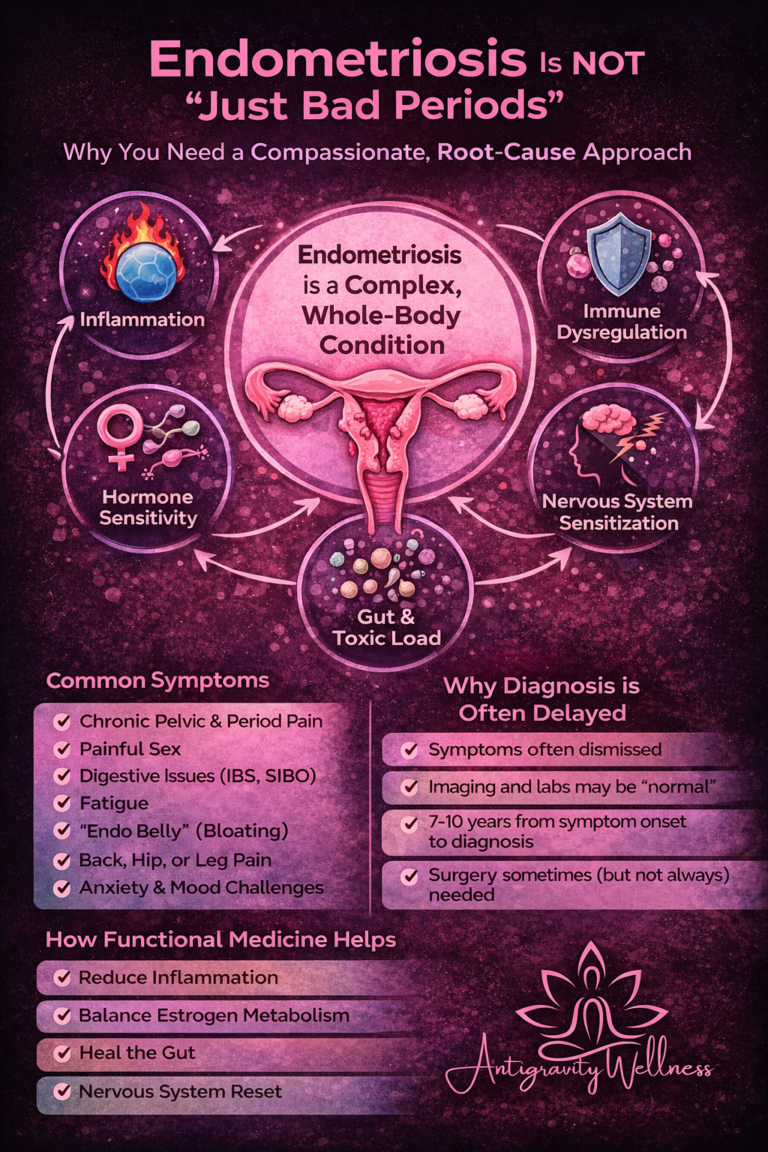
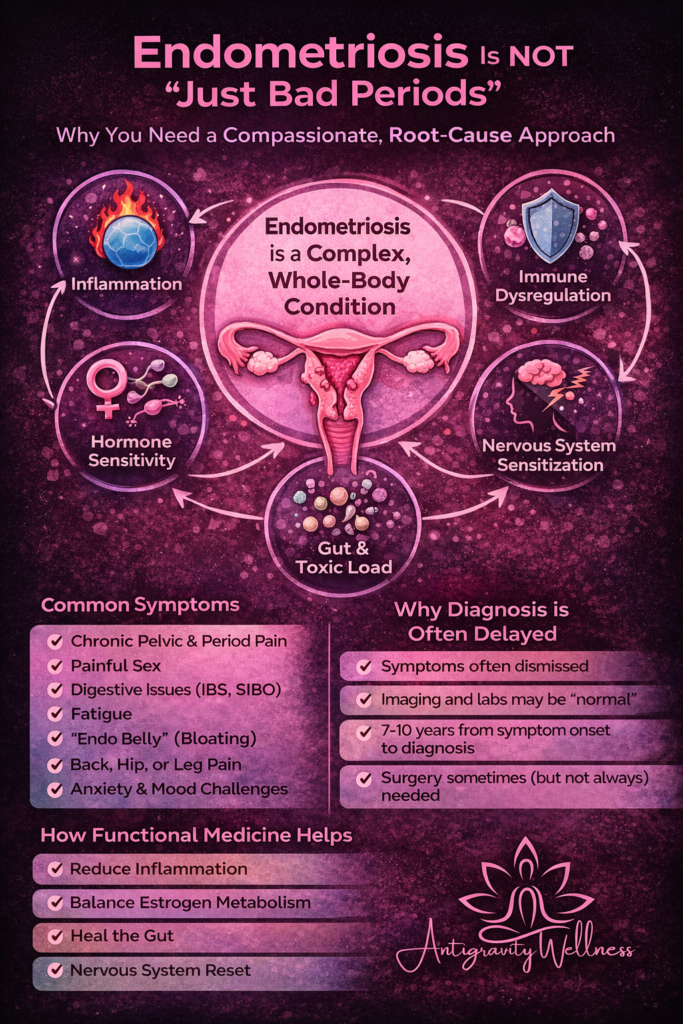
Endometriosis Is a Whole-Body Condition—Not Just a Gynecologic One
Endometriosis is traditionally defined as tissue similar to the uterine lining growing outside the uterus. But modern research shows that it is far more complex than misplaced tissue.
Endometriosis is best understood as a chronic inflammatory, immune-mediated, hormone-sensitive condition that affects multiple systems, including:
- The immune system
- The nervous system
- Estrogen metabolism
- Gut and liver function
- Pain signaling pathways
This is why symptoms often extend far beyond the pelvis.
Common Symptoms of Endometriosis (That Often Get Missed)
While pelvic pain and painful periods are common, endometriosis may also present as:
- Pain with ovulation or bowel movements
- Chronic low back or hip pain
- Pain with intercourse
- Fatigue that doesn’t improve with rest
- Bloating (“endo belly”)
- IBS-like symptoms
- Migraines or headaches
- Anxiety or depression related to chronic pain
- Fertility challenges
👉 Many women are told these symptoms are unrelated—when they are often connected by the same underlying drivers.
Why Endometriosis Is So Hard to Diagnose
Unlike PCOS, there is no single blood test or ultrasound that can reliably diagnose endometriosis.
- Imaging may be completely normal
- Labs may look “fine”
- Symptoms can fluctuate over time
- Pain severity does not always match disease extent
The gold standard diagnosis remains laparoscopic surgery, but many women never reach that step—or are told surgery isn’t warranted despite ongoing symptoms.
📌 This leads to delayed care and symptom management rather than meaningful intervention.
Endometriosis Is Also a Spectrum Condition
Endometriosis does not look the same in every woman.
Some experience severe pain with minimal visible disease.
Others have extensive disease with fewer symptoms.
From a functional medicine perspective, endometriosis exists on a spectrum of dominant drivers, including:
- Chronic inflammation
- Immune dysregulation
- Estrogen dominance or impaired estrogen clearance
- Nervous system sensitization
- Gut dysfunction
- Genetic susceptibility
Understanding which drivers are most active is key to effective treatment.
Why Conventional Treatment Often Falls Short
Standard care for endometriosis typically focuses on:
- Hormonal suppression (birth control, GnRH analogs)
- Pain management
- Surgical excision when severe
These options can be helpful—and sometimes necessary—but they often:
- Do not address underlying inflammation or immune drivers
- Do not prevent recurrence
- Do not support whole-body healing
- Leave women feeling dependent on medication alone
This is where many patients feel stuck:
“I don’t want to just keep suppressing my symptoms, but I don’t know what else to do.”
How Functional Medicine Approaches Endometriosis Differently
Functional medicine doesn’t ask:
“How do we shut this down?”
It asks:
“Why is this happening in the first place?”
At Antigravity Wellness, we evaluate endometriosis through a whole-body lens, including:
- Inflammatory markers
- Estrogen metabolism and detoxification pathways
- Gut health and microbiome balance
- Nutrient deficiencies
- Stress and nervous system regulation
- Metabolic health
- Lifestyle contributors that amplify pain signaling
Treatment plans may include:
- Anti-inflammatory, hormone-supportive nutrition
- Gut healing protocols
- Stress and nervous system regulation
- Targeted supplementation
- Movement strategies that support—not worsen—symptoms
- Medication when appropriate, but not as the sole solution
Case Study #1: “I Was Told My Pain Was Normal”
“I thought maybe I just had a low pain tolerance.”
Emily, 29, had painful periods since her teens. Over time, the pain worsened and began affecting her digestion, energy, and ability to work.
Her ultrasounds were normal.
Her labs were “fine.”
She was repeatedly offered birth control.
At Antigravity Wellness, we identified:
- Significant inflammatory signaling
- Estrogen metabolism imbalance
- Gut dysfunction contributing to immune activation
“For the first time, someone connected all the dots instead of treating each symptom separately.”
Within her first phase of care, Emily began experiencing less pain, improved energy, and fewer flares, with a clear long-term strategy that didn’t rely on symptom suppression alone.
Case Study #2: Endometriosis in Perimenopause
“I thought this would get better as I got older.”
Rachel, 44, came in with worsening pelvic pain, bloating, fatigue, and irregular cycles as she entered perimenopause.
She assumed endometriosis no longer applied.
Instead, hormonal shifts had amplified underlying inflammation and nervous system sensitivity.
“I finally understood why everything felt worse—not better.”
By addressing inflammation, estrogen clearance, stress physiology, and metabolic health together, she saw meaningful improvements in quality of life—without chasing symptoms one by one.
Endometriosis Deserves Better Than Symptom Suppression
Endometriosis is not:
❌ “Just bad periods”
❌ A condition you have to suffer through
❌ Something that only affects fertility
It is a complex, whole-body condition that deserves individualized, compassionate care.
How Antigravity Wellness Supports Endometriosis Patients
We work with patients to:
- Identify dominant drivers of symptoms
- Reduce inflammation and immune activation
- Support hormone balance safely
- Improve pain, energy, and quality of life
- Create sustainable, realistic treatment plans aligned with personal goals
If you’re wondering whether our functional approach is right for you, we invite you to start with our Readiness Questionnaire to explore next steps.
Medical Disclaimer
This content is for educational purposes only and does not constitute medical advice. Diagnosis and treatment should always be individualized and discussed with a qualified healthcare provider.
References
- Zondervan KT et al. Endometriosis. N Engl J Med. 2020. https://www.nejm.org/doi/full/10.1056/NEJMra1810764
- Bulun SE. Endometriosis. N Engl J Med. 2009. https://www.nejm.org/doi/full/10.1056/NEJMra0804690
- Vercellini P et al. Endometriosis: pathogenesis and treatment. Lancet. 2014. https://pubmed.ncbi.nlm.nih.gov/24366116/
- Giudice LC. Clinical practice: Endometriosis. N Engl J Med. 2010. https://pubmed.ncbi.nlm.nih.gov/20573927/