The Wake-Up Call Many Women Don’t Expect
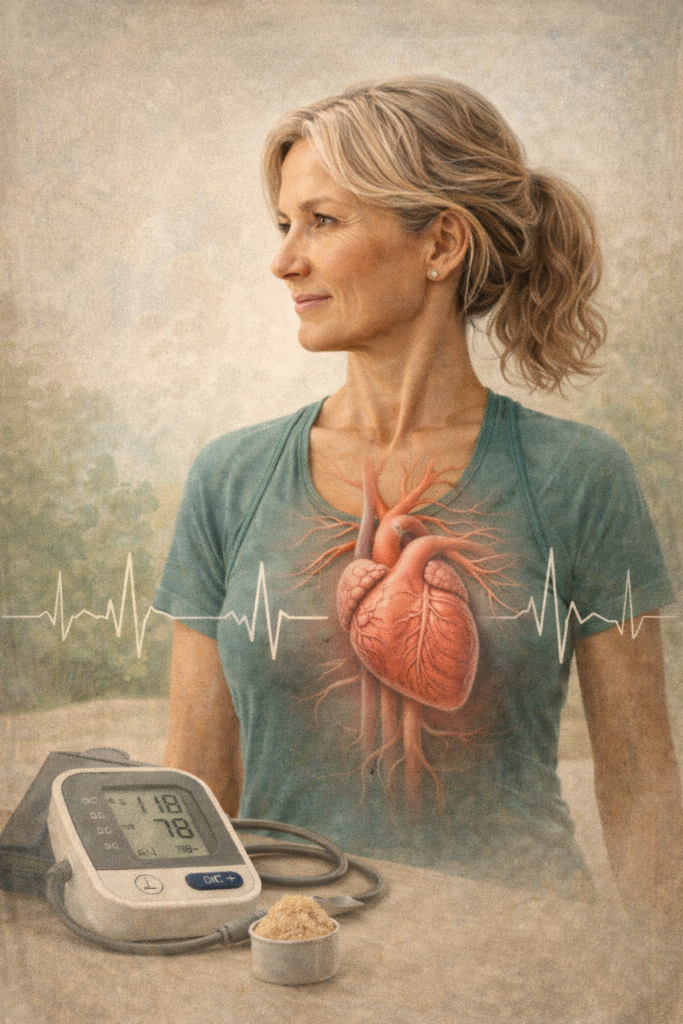
She came in thinking she was just “getting older.”
She was 44.
Busy. Active. Eating well. Exercising regularly.
But over the last year, she noticed she was more tired than usual. Her workouts felt harder. Her heart would race at times. Her blood pressure—once perfect—was creeping up.
Her labs were still “normal,” so she was told everything was fine.
But her body was telling a different story.
This is a situation I see every week—and it often starts during perimenopause, the hormone transition that happens before menopause.
Why Heart Risk Increases After 40
Heart disease is the leading cause of death in women.
Yet many women don’t realize their risk begins to rise before menopause, not after.
The Estrogen Connection (Explained Simply)
Estrogen is a hormone that does more than control periods.
It helps:
- Keep blood vessels flexible
- Support healthy cholesterol
- Reduce inflammation (swelling inside the body)
- Improve blood flow to the heart
During perimenopause, estrogen levels become unpredictable. Some days they’re high. Some days they’re low. Over time, they trend downward.
As estrogen protection fades, the heart becomes more vulnerable.
Heart Symptoms in Women Often Look Different
Women don’t always have the “classic” crushing chest pain seen in men.
Common heart-related symptoms in women include:
- Ongoing fatigue
- Shortness of breath
- Heart racing or fluttering (palpitations)
- Chest tightness or pressure
- Anxiety-like feelings
- Poor exercise tolerance
These symptoms are often dismissed as stress, anxiety, or aging—especially during perimenopause.
They shouldn’t be.
Other Factors That Increase Heart Risk in Perimenopause
Hormone changes don’t happen in isolation. They affect many systems at once.
Common contributors include:
- Insulin resistance (difficulty controlling blood sugar)
- Visceral fat (fat around the organs)
- Chronic stress and high cortisol (stress hormone)
- Poor sleep quality
- Over-exercising or under-recovering
All of these increase strain on the heart.
The Role of Exercise (More Isn’t Always Better)
Exercise is one of the best tools for heart health—but only when done correctly.
Heart-supportive movement includes:
- Strength training (builds muscle and improves blood sugar control)
- Walking or steady cardio (supports blood pressure and endurance)
- Short bursts of intensity (when appropriate)
- Recovery and rest (lowers stress hormones)
Too much cardio or intense training without recovery can raise cortisol, which increases heart strain—especially in perimenopause.
Nutrition Matters More Than Calories
Extreme dieting is common in midlife women—and it backfires.
Heart-supportive nutrition focuses on:
- Adequate protein
- Fiber-rich vegetables and fruits
- Healthy fats (especially omega-3s)
- Balanced meals to stabilize blood sugar
Chronic under-eating and blood sugar swings increase heart risk.
Stress Is a Major Heart Risk for Women
Stress affects women’s hearts more than men’s.
High stress can:
- Raise blood pressure
- Increase inflammation
- Disrupt heart rhythm
- Increase abdominal fat
This happens through cortisol, the body’s main stress hormone.
Stress care is not optional.
It is heart care.
Case Study: Catching Risk Early
A 46-year-old woman came to Antigravity Wellness feeling exhausted and frustrated.
Her labs were “normal,” but trends showed:
- Rising blood pressure
- Lower HDL (“good”) cholesterol
- Increased belly fat
- Poor sleep and high stress
She was in perimenopause.
By addressing:
- Hormone balance
- Strength-based exercise
- Blood sugar stability
- Stress and recovery
She saw improvements in energy, workouts, labs, and confidence—without extreme dieting or over-training.
Early intervention changed her long-term heart risk.
How Antigravity Wellness Supports Women’s Heart Health
At Antigravity Wellness, we take a whole-woman, hormone-aware approach.
Our care packages focus on:
- Identifying early cardiovascular risk
- Understanding hormone shifts
- Optimizing lifestyle, nutrition, and movement
- Supporting stress and sleep
- Monitoring trends—not just “normal” ranges
We don’t wait for disease.
We focus on prevention and resilience.
How to Work With Us
The first step is our Readiness Questionnaire, which helps determine:
- Whether our care is the right fit
- What level of support you may need
- Your next best step forward
👉 Take the Readiness Questionnaire here
You Deserve Proactive Care
Perimenopause is not the beginning of decline.
It is a window of opportunity to protect your heart, energy, and long-term health.
With the right support, women can feel stronger after 40—not worse.
Medical References
- American Heart Association. Heart Disease and Stroke Statistics. https://www.ahajournals.org/doi/10.1161/CIR.0000000000001412
- Menopause And Cardiovascular Disease. https://www.utphysicians.com/normalizing-menopause-and-its-association-with-cardiovascular-disease/
- Risks, Benefits, and Treatment Modalities of Menopausal Hormone Therapy. https://pmc.ncbi.nlm.nih.gov/articles/PMC8034540/
- Women and heart disease, the underrecognized burden. https://pubmed.ncbi.nlm.nih.gov/26957643/
- Visceral Adiposity and Cardiometabolic Risk. https://pubmed.ncbi.nlm.nih.gov/40622164/
Medical Disclaimer
This blog is for educational purposes only and does not replace individualized medical advice. Always consult a qualified healthcare provider before making changes to your health plan, medications, supplements, or exercise routine.