Carrie, 41, had started planning her day around the bathroom. Some mornings she’d wake up with stabbing cramps and need to run to the toilet—other days, she’d go three days without a single bowel movement. Every meal felt like a gamble: will this make me bloat, cramp, or need to leave a meeting early? She’d been told it was “just IBS,” but the label didn’t help. It didn’t explain why her symptoms flared around her period or why her energy and mood crashed when her gut was off.
Carrie wanted real answers—and a plan that didn’t just involve more fiber or guesswork.
What Is IBS?
Irritable Bowel Syndrome (IBS) is a functional GI disorder, which means the digestive tract looks normal on imaging, but isn’t functioning properly. IBS is defined by:
- Abdominal pain or discomfort at least once per week
- Changes in bowel habits (constipation, diarrhea, or both)
- Relief or worsening of symptoms after bowel movements
IBS is classified into subtypes:
- IBS-D (diarrhea-predominant)
- IBS-C (constipation-predominant)
- IBS-M (mixed)
While it affects both men and women, IBS is twice as common in women—and symptoms often worsen during perimenopause and menopause.
Why IBS Flares During Perimenopause and Menopause
Hormones, stress, and gut function are all closely linked. During your 30s, 40s, and 50s, fluctuating estrogen and progesterone levels affect digestion in powerful ways:
- Low progesterone slows motility, contributing to constipation
- Estrogen fluctuations influence bile production, microbiome balance, and gut inflammation
- Cortisol dysregulation from chronic stress impacts gut-brain signaling and motility [^1]
- Thyroid function, which often changes midlife, can mimic or worsen IBS symptoms
Many women experience gut changes right before their period—loose stools, cramps, or bloating—and these patterns often become more intense in perimenopause.
Common Risk Factors for IBS
IBS isn’t caused by one thing—it’s a syndrome with many possible triggers. Here are some of the key risk factors we assess at Antigravity Wellness:
- History of food poisoning or GI infections (can damage gut nerves)
- Gallbladder removal (changes fat digestion and bile regulation)
- Chronic stress or trauma, especially unprocessed emotional stress
- Frequent antibiotic use, which disrupts the microbiome
- Long-term acid-blocker or NSAID use
- Hormonal contraceptive use
- Small Intestinal Bacterial Overgrowth (SIBO) or other gut imbalances
- Undiagnosed hypothyroidism or Hashimoto’s disease
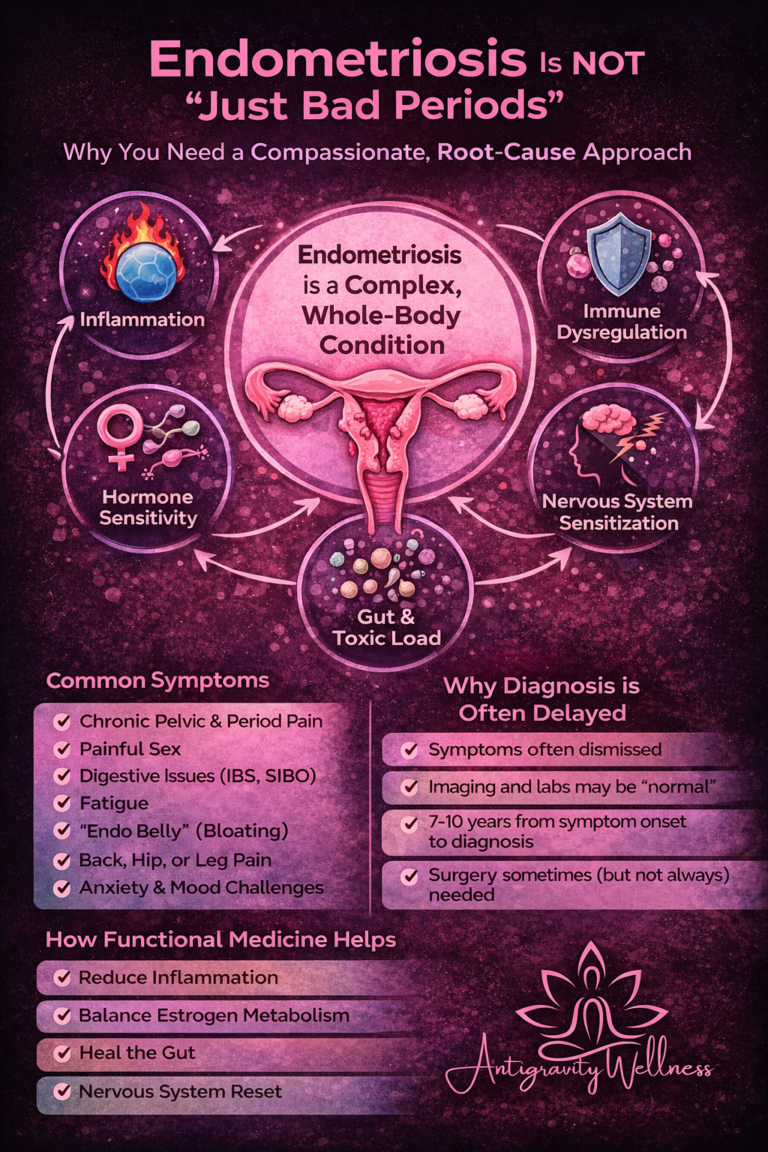
- Endometriosis or pelvic surgery, which can affect gut motility
If these sound familiar, your IBS might have a clear root cause—one that hasn’t been identified yet.
When to Seek More Than a Diagnosis
IBS is often diagnosed by exclusion. But it’s important to rule out serious conditions like:
- Inflammatory Bowel Disease (Crohn’s, ulcerative colitis)
- Celiac disease
- Colon cancer
- Microscopic colitis
- Endometriosis
Red flags that warrant further testing include:
- Blood in stool
- Nighttime symptoms that wake you up
- Unintentional weight loss
- Iron-deficiency anemia
At Antigravity Wellness, we don’t stop at “IBS.” We use advanced functional testing, like:
- The GI MAP stool test to evaluate microbiome health, inflammation, enzyme output, and gut pathogens
- SIBO breath testing
- DUTCH hormone testing to assess cortisol, estrogen, and progesterone patterns
- Thyroid and adrenal panels
- Food sensitivity testing, when appropriate
This testing helps us personalize treatment—so you stop guessing and start healing.
Holistic Strategies for IBS Relief
Whether you deal with IBS-C, IBS-D, or a mix of both, we approach healing from the inside out:
✅ Nervous System Regulation
- Vagal nerve exercises (like gargling, humming, or cold exposure)
- Breathwork and gentle movement (yoga, walking)
- Somatic tools to release stress stored in the body
✅ Nutrition Strategies
- Short-term elimination diets, such as low-FODMAP, may reduce symptoms
- Identify and eliminate trigger foods: dairy, gluten, soy, alcohol, and caffeine are common culprits
- Cooked, easy-to-digest meals reduce gut workload
- Reintroduce foods slowly, with guidance, to prevent unnecessary restriction
✅ Targeted Supplements
- Digestive enzymes and bitters to support digestion
- L-glutamine and zinc carnosine for gut lining repair
- PHGG or acacia fiber to improve stool consistency without bloating
- Specific probiotics matched to your microbiome needs (after testing)
We carry practitioner-vetted products in our Fullscript Supplement Shop, but always confirm compatibility with your provider.
Conventional Medical Options
Conventional treatments for IBS may include:
- Antispasmodics for cramping
- Antidiarrheal or laxative medications
- SSRIs or tricyclic antidepressants for gut-brain signaling
- Prescription meds like linaclotide (for IBS-C) or rifaximin (for IBS-D/SIBO overlap)
These may help in the short term, but without root-cause care, many women find their symptoms return—or shift into something new.
Case Study: Meet Renee
Renee, 46, came to Antigravity Wellness after 15 years of being told she “just had IBS.” Her symptoms worsened during perimenopause—more bloating, unpredictable bowel movements, and constant fatigue.
We ran a GI MAP and DUTCH test, uncovering:
- Dysbiosis and low beneficial flora
- Poor estrogen clearance
- Low cortisol in the morning and elevated cortisol at night
She began a personalized protocol that included:
- A 4-week gut repair plan with antimicrobials, digestive enzymes, and probiotics
- A low-FODMAP reset followed by gentle food reintroduction
- Daily breathwork and nervous system retraining
- Bioidentical progesterone support
In just 8 weeks, Renee’s bloating and fatigue improved dramatically, and she was having regular, pain-free bowel movements for the first time in years.
Why IBS Deserves More Than a Shrug
IBS isn’t “just in your head.” It’s a real, complex, body-wide syndrome that affects your digestion, hormones, mood, energy, and quality of life. And if you’re in perimenopause, your gut symptoms are not separate from your hormonal symptoms—they’re speaking the same language.
The good news? When we treat the root causes with precision, your gut can heal—and your life gets better in the process.
Let’s Work Together to Rebuild Trust With Your Body
At Antigravity Wellness, we don’t just manage IBS—we help you understand it. We use cutting-edge testing, customized nutrition, nervous system care, and hormone balancing to restore your rhythm.
Are you ready to stop fearing food, bathrooms, and your own body?
👉 Book your Brief Initial Consult now
👉 Explore our favorite gut and hormone support supplements in the Fullscript Shop
Resources and References
- Chang L, et al. “Gender, age, society, culture, and the patient’s perspective in the functional gastrointestinal disorders.” Gastroenterology. 2006;130(5):1435–1446. https://doi.org/10.1053/j.gastro.2005.09.071
- Rees WD, et al. “The role of sex hormones in gastrointestinal function and disease.” Gastroenterol Hepatol Bed Bench. 2022;15(1):3–13. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8804275/
- Efficacy of Dietary Interventions for Irritable Bowel Syndrome: A Systematic Review and Network Meta-Analysis. https://pmc.ncbi.nlm.nih.gov/articles/PMC11728101/