
Probiotics, Prebiotics, and Women’s Hormonal Health: The Triad of Gut Balance
Probiotics, Prebiotics, and Women’s Hormonal Health: The Triad of Gut Balance When it comes to women’s health, hormonal balance plays a pivotal role. From regulating
While progesterone is thought of as primarily a uterus hormone essential for getting a pregnancy to term, its role in how a woman feels and functions does not stop with childbearing years or post-hysterectomy, contrary to what some Western Medicine doctors have been taught.
In this blog, I will review what progesterone is, why postmenopausal women still need progesterone, how progesterone affects mood and sleep, how to support progesterone in the postmenopausal woman naturally, and what supplements can help with progesterone. menopausal Woman:
Progesterone is a hormone that plays a crucial role in the female reproductive system. It is one of the two main hormones involved in the menstrual cycle and is primarily produced by the ovaries in women. Smaller amounts of progesterone are also produced by the adrenal glands (the primary source in postmenopausal women) and the placenta during pregnancy.
Progesterone helps prepare the uterus for pregnancy and is involved in regulating the menstrual cycle. During the menstrual cycle, progesterone levels rise after ovulation and help thicken the uterine lining in preparation for the implantation of a fertilized egg. If pregnancy occurs, progesterone continues to be produced to support the development of the embryo and maintain the uterine lining.
If pregnancy does not occur, progesterone levels decline, leading to the shedding of the uterine lining and the start of a new menstrual cycle. In addition to its role in the menstrual cycle, progesterone also plays a part in maintaining a healthy pregnancy by inhibiting contractions of the uterus and supporting the growth of the placenta.
Progesterone is also used medically for various purposes. It is commonly prescribed as part of hormone replacement therapy (HRT) to relieve symptoms of menopause and to support the endometrium (uterine lining) in women receiving estrogen replacement therapy. Progesterone can also be prescribed to help regulate irregular menstrual cycles and treat conditions such as endometriosis and infertility.
It’s important to note that while progesterone is primarily associated with female reproductive functions, it is also produced in smaller amounts in males and plays a role in certain physiological processes, such as sperm production.
Why would a post-menopausal woman need progesterone?
In postmenopausal women, the need for progesterone may vary depending on individual circumstances and health conditions. While postmenopausal women no longer experience menstrual cycles or require progesterone for fertility purposes, there are certain situations where progesterone may still be recommended. Here are a few scenarios where progesterone may be prescribed for postmenopausal women:
It’s important to note that the decision to use progesterone in postmenopausal women should be made on an individual basis, taking into consideration factors such as personal health history, symptoms, and potential risks and benefits. It is recommended to consult with a healthcare professional who specializes in menopause management or hormone therapy to discuss the specific needs and considerations in your situation.
How does progesterone affect mood?
Progesterone can have various effects on mood due to its influence on the central nervous system and interactions with neurotransmitters in the brain. Here are some ways in which progesterone can impact mood:
It’s important to note that the effects of progesterone on mood can vary among individuals and can be influenced by factors such as hormone levels, fluctuations throughout the menstrual cycle, and individual sensitivity to hormonal changes. Additionally, progesterone’s effects on mood may be more noticeable in women with hormone imbalances or those experiencing fluctuations in hormone levels, such as during the menstrual cycle or perimenopause.
If you are experiencing significant mood changes or concerns about your mood, it is advisable to consult with a healthcare professional, such as a gynecologist or endocrinologist, who can evaluate your specific situation, assess hormone levels if necessary, and provide appropriate guidance and treatment options.
How does progesterone affect sleep?
Progesterone can influence sleep in several ways due to its effects on the central nervous system and interactions with neurotransmitters. Here are some ways in which progesterone can affect sleep:
It’s important to note that the effects of progesterone on sleep can vary among individuals and can be influenced by factors such as hormone levels, fluctuations throughout the menstrual cycle, and individual sensitivity to hormonal changes. Additionally, other factors, such as lifestyle habits, stress, and underlying sleep disorders, can also impact sleep quality.
If you are experiencing persistent sleep disturbances or concerns about your sleep patterns, it is advisable to consult with a healthcare professional who can evaluate your specific situation, assess hormone levels if necessary, and provide appropriate guidance and treatment options. They can help determine if progesterone supplementation or other interventions are suitable for your individual needs.
How to naturally support progesterone in the postmenopausal woman.
In postmenopausal women, the production of progesterone naturally declines due to the cessation of ovarian function. While it may not be possible to restore progesterone levels to pre-menopausal levels naturally, there are lifestyle changes and natural remedies that may help support hormonal balance and overall well-being. Here are some strategies that may assist in naturally supporting progesterone levels in postmenopausal women:
Remember, it is always recommended to consult with a healthcare professional who specializes in hormone health and menopause before making any significant changes to your diet, lifestyle, or considering hormone therapy. They can provide personalized guidance based on your individual needs and medical history.
What supplements can help support a healthy progesterone level in a postmenopausal woman?
In postmenopausal women, progesterone levels naturally decline due to the cessation of ovarian function. While there are no specific supplements that can directly increase progesterone levels, some supplements and nutrients may support hormonal balance and overall well-being. It’s important to note that individual responses to supplements may vary, and it’s recommended to consult with a healthcare professional before starting any new supplements. Here are some supplements that are sometimes used to support hormonal balance in postmenopausal women:
Remember that supplements should not replace a balanced diet and a healthy lifestyle. They are intended to complement a well-rounded approach to overall health and hormonal balance. It’s important to work with a healthcare professional who can evaluate your specific needs, assess any potential deficiencies, and provide personalized recommendations based on your individual health status and goals.
Need your hormones checked? Can’t get your doctor to take you seriously? Tired of the sick approach to your health? Contact me at Antigravity Wellness today.
Deeper Dive: Check out this review if you want to learn more about progesterone in peri- and postmenopause:
Regidor PA. Progesterone in Peri- and Postmenopause: A Review. Geburtshilfe Frauenheilkd. 2014 Nov;74(11):995-1002. doi: 10.1055/s-0034-1383297. PMID: 25484373; PMCID: PMC4245250.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4245250/

Hi! My name is Nicole D. Smith, and I am a Doctorally prepared Advanced Registered Family Nurse Practitioner in Washington State. I specialize in Functional Nutrition, Fitness, and Medicine, as well as Women’s Health, Hormones, and Metabolism. You can set up a consult with me here. I would love to help you get to the root cause of why you are not feeling and looking your best so we can work together to get you back to feeling more energetic, youthful, leaner, and stronger than you thought possible!

Probiotics, Prebiotics, and Women’s Hormonal Health: The Triad of Gut Balance When it comes to women’s health, hormonal balance plays a pivotal role. From regulating
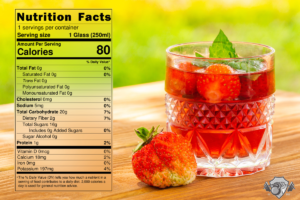
INGREDIENTS (1 serving) 10 minutes Directions Nutrition per serving Calories 79 Carbs 20g Protein 1g Fats 0g Sodium 6mg

Hello! Nurse Practitioner, Functional Nutrition & Fitness Coach Nicole here to talk to you about 4 tactics that night shift workers can implement to optimize