Protein gets all the attention.
Carbs get all the blame.
Fat gets all the debate.
But the nutrient that quietly determines gut health, hormone balance, metabolic health, brain health, and cardiovascular risk in midlife women?
Fiber.
And most women are getting nowhere near enough—especially during perimenopause and menopause, when fiber becomes even more critical.
Let’s talk about why fiber matters, how hormones affect the gut, what the research actually shows, and what this looks like in real life—not just on paper.
___________________________________________________________________________
Fiber needs increase in midlife—and the bar is higher than you think
The American Heart Association now recommends at least 30–35 grams of fiber per day for women, specifically for:
Heart health
Gut health
Blood sugar regulation
Cholesterol management
Most women average 10–15 grams per day.
That gap matters—especially in perimenopause.
___________________________________________________________________________
Why fiber is especially important in perimenopause & menopause
1️⃣ Estrogen directly affects the gut
As estrogen declines:
Gut motility slows
The microbiome shifts
Constipation becomes more common
Bloating and gas increase
Estrogen detoxification becomes less efficient
Fiber plays a key role in:
Binding estrogen in the gut
Supporting healthy elimination
Preventing estrogen recirculation
Reducing systemic inflammation
Low fiber = hormonal traffic jam.
2️⃣ The gut–brain axis becomes more sensitive
The gut and brain communicate constantly through:
The vagus nerve
Neurotransmitters (like serotonin—90% of which is made in the gut)
Inflammatory signaling
Poor gut health in midlife is linked to:
Anxiety
Mood changes
Brain fog
Sleep disruption
Fiber feeds the bacteria that produce short-chain fatty acids (SCFAs)—key compounds that reduce inflammation and support brain health.
3️⃣ Fiber protects the heart, metabolism, and liver
Adequate fiber intake:
Improves insulin sensitivity
Lowers LDL cholesterol
Reduces cardiovascular risk
Supports liver detoxification pathways
This is especially important as women lose estrogen’s cardioprotective effects after menopause.
___________________________________________________________________________
Soluble vs insoluble fiber: what’s the difference?
Both matter—but they do different jobs.
Soluble fiber
Dissolves in water
Forms a gel-like substance
Slows digestion
Feeds beneficial gut bacteria
Helpful for:
Diarrhea
Blood sugar swings
Cholesterol reduction
IBS with loose stools
Sources:
Oats
Chia seeds
Flaxseed
Beans and lentils
Psyllium
Some fruits (apples, berries)
___________________________________________________________________________
Insoluble fiber
Does not dissolve in water
Adds bulk to stool
Speeds intestinal transit
Helpful for:
Constipation
Sluggish digestion
Sources:
Vegetables
Whole grains
Nuts and seeds
Fruit skins
Most women need both—but the ratio matters depending on symptoms.
___________________________________________________________________________
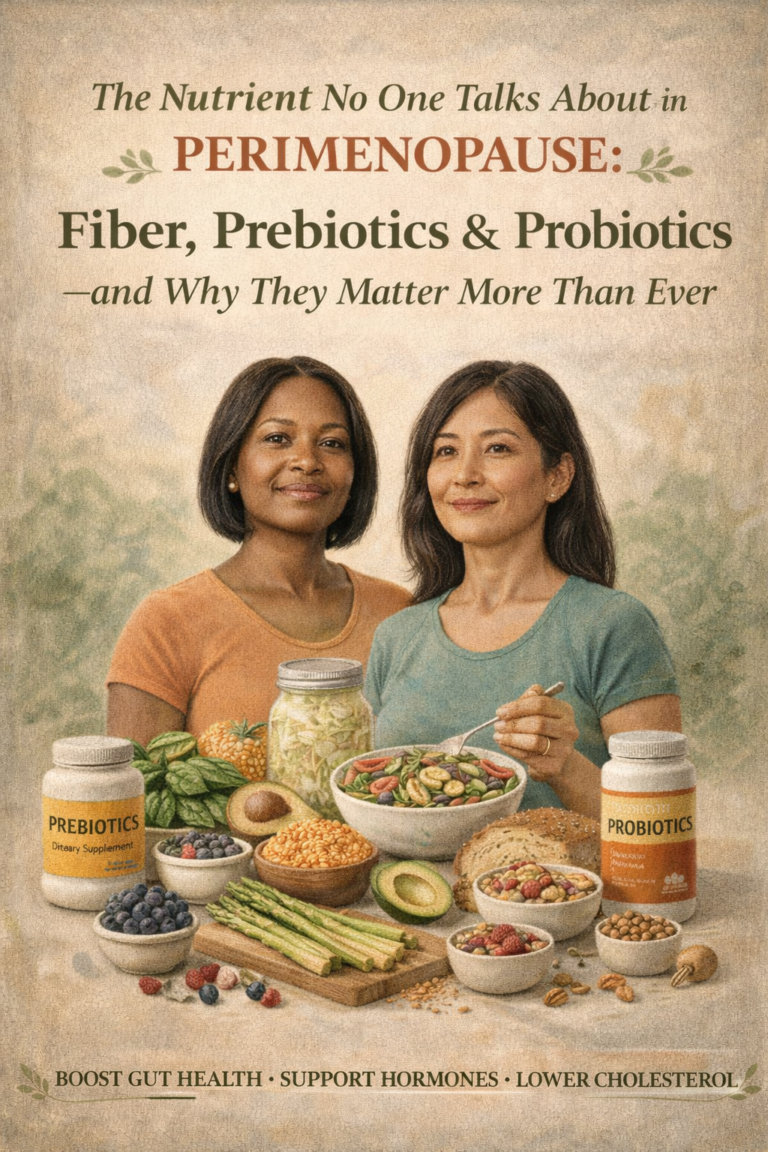
Prebiotic vs probiotic foods (they are not the same)
Prebiotics = food for your gut bacteria
Prebiotic fibers selectively feed beneficial microbes.
Examples:
Onions
Garlic
Leeks
Asparagus
Artichokes
Green bananas
Oats
Chicory root
No prebiotics = probiotics can’t thrive.
___________________________________________________________________________
Probiotics = the bacteria themselves
Probiotic foods introduce beneficial organisms.
Examples:
Yogurt (dairy-free options count)
Kefir
Sauerkraut
Kimchi
Miso
Tempeh
Both matter—but prebiotics are often the missing piece.
___________________________________________________________________________
What 30–35 grams of fiber actually looks like in a day
This is where things click 👇
Breakfast
Chia pudding (2 Tbsp chia): ~10 g
Blueberries (1 cup): ~4 g
Lunch
Large salad with mixed greens, veggies, chickpeas (½ cup): ~8–10 g
Snack
Apple with skin: ~4 g
Handful of almonds: ~3 g
Dinner
Roasted vegetables (2 cups): ~6–8 g
👉 Total: 30–35 grams
No extremes. No deprivation. Just intentional choices.
___________________________________________________________________________
When food alone isn’t enough: fiber supplements
Sometimes food isn’t sufficient—especially if:
Constipation or diarrhea is significant
Appetite is low
GI symptoms limit food variety
Fiber intake needs to increase slowly
One supplement we commonly use and recommend in practice is Thorne FiberMend.
Why FiberMend works well
Blend of soluble and insoluble prebiotic fibers
Gentle and well tolerated
Supports both constipation and diarrhea
Feeds beneficial gut bacteria
Non-stimulant (not habit-forming)
This kind of fiber supports normalization, not forcing bowel movements.
___________________________________________________________________________
A critical caution about laxatives (especially long-term use)
Chronic use of laxatives—especially osmotic agents like Miralax—can:
Reduce gut motility over time
Create dependency
Mask underlying problems
Make it harder to have normal bowel movements without them
Many women are told to “just take it forever.”
That’s not a solution—it’s a band-aid.
If laxatives are needed short-term, they should be used strategically and under guidance, while addressing root causes.
___________________________________________________________________________
Constipation and diarrhea are symptoms—not diagnoses
Chronic GI symptoms often point to underlying issues, including:
Thyroid dysfunction (especially hypothyroidism)
Hormonal imbalance
Iron deficiency
Gut dysbiosis
Food intolerances
Nervous system dysregulation
Many women with long-standing constipation later discover undiagnosed thyroid disease—something that was dismissed for years.
Just because you’ve “always had it” does not mean it’s normal.
___________________________________________________________________________
Why estrogen loss affects the gut (and why this matters)
As estrogen declines:
Gut barrier function weakens
Motility slows
Microbial diversity decreases
Inflammation increases
This impacts:
Digestion
Mood
Immune function
Liver detoxification
Hormone metabolism
Supporting the gut during perimenopause is not optional—it’s foundational.
___________________________________________________________________________
The big picture: gut health, hormones, brain, and liver are connected
Fiber sits at the center of:
Hormone detoxification
Neurotransmitter production
Inflammation control
Cardiovascular protection
Ignoring gut symptoms because they’re “embarrassing” allows problems to worsen quietly.
Seeking care from a functional provider who looks for why—not just what—is wrong can be life-changing.
___________________________________________________________________________
How This Fits Into Care at Antigravity Wellness
At Antigravity Wellness, we:
Take gut symptoms seriously
Evaluate thyroid and hormone contributors
Address nutrition, stress, and motility
Use supplements strategically—not reflexively
Avoid symptom suppression without understanding root cause
Fiber is not “just a digestive issue.”
It’s a core pillar of midlife health and vitality.
___________________________________________________________________________
Are We a Good Fit?
If you’re dealing with:
Chronic constipation or diarrhea
Bloating and gas
Hormone-related GI changes
Confusion about what to eat
👉 Take the Readiness Questionnaire to explore whether our whole-person approach aligns with your goals.
___________________________________________________________________________
References
1. American Heart Association. Dietary Guidance to Improve Cardiovascular Health. https://www.ahajournals.org/doi/10.1161/cir.0000000000001031
2. Slavin, J. L. (2013).
Fiber and prebiotics: Mechanisms and health benefits.
Nutrients, 5(4), 1417–1435. https://pubmed.ncbi.nlm.nih.gov/23609775/
3. Makki, K., et al. (2018).
The impact of dietary fiber on gut microbiota.
Cell Host & Microbe, 23(6), 705–715. https://pubmed.ncbi.nlm.nih.gov/29902436/
4. Simpson, H. L., & Campbell, B. J. (2015).
Review article: Dietary fibre–microbiota interactions.
Alimentary Pharmacology & Therapeutics, 42(2), 158–179. https://pubmed.ncbi.nlm.nih.gov/26011307/
5. Gut microbiota changes in menopause. https://tinyurl.com/2jeyhvbf
___________________________________________________________________________
Medical Disclaimer
This article is for educational purposes only and does not constitute medical, nutritional, or supplement advice. Individual needs vary. Always consult a qualified healthcare provider before starting new supplements, medications, or dietary interventions.