Jessica, 38, had lived with painful periods since her teens. Every month she’d miss work, cancel plans, and curl up with a heating pad while trying not to cry. Her doctor told her it was “just part of being a woman,” and she believed it—until the pain started creeping in even when she wasn’t menstruating. Now in her late 30s, Jessica also felt more fatigued, bloated, and inflamed than ever. Sex had become uncomfortable. Her digestion was erratic. Her PMS was brutal. She didn’t know what was happening, but she knew this wasn’t “normal.”
What Is Endometriosis?
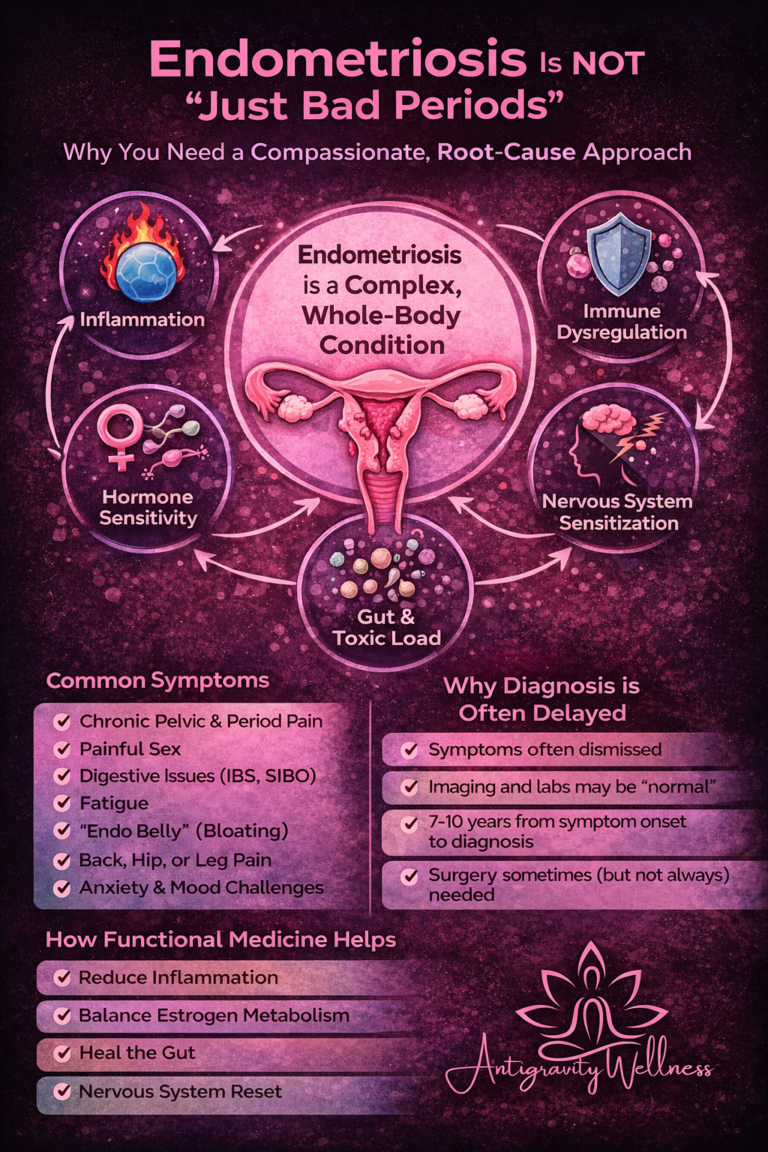
Endometriosis is a chronic inflammatory condition where tissue similar to the lining of the uterus (endometrium) grows outside the uterus—on the ovaries, fallopian tubes, bladder, bowels, and even the pelvic wall.
These endometrial-like cells respond to hormonal signals, especially estrogen, but since they’re located outside the uterus, they can’t exit the body like menstrual blood. This leads to:
- Inflammation
- Scar tissue
- Adhesions
- Pain and dysfunction in nearby organs
Endometriosis affects at least 1 in 10 women, and many are misdiagnosed or dismissed for years. Symptoms can start in adolescence and often worsen in the 30s and 40s.
Why Endometriosis Often Gets Worse with Age and Hormone Shifts
Perimenopause is a time of hormonal turbulence, and for women with endometriosis, it can feel like a perfect storm:
- Estrogen levels fluctuate, but remain high relative to low progesterone, a state known as estrogen dominance.
- Estrogen fuels endometrial tissue growth and inflammation.
- Progesterone’s anti-inflammatory, anti-growth effects are missing or insufficient, allowing symptoms to worsen.
- Cortisol imbalances due to stress make inflammation and pain sensitivity worse.
- Poor gut function and detoxification pathways may reduce the body’s ability to eliminate excess estrogen.
Many women are told that their endometriosis will improve after menopause, but this isn’t always true—especially if they have high body fat (which produces estrogen), are on estrogen-only therapy, or have residual inflammation and scarring.
Common Risk Factors for Endometriosis
While the exact cause is still debated, research suggests several contributing factors:
- Genetics and family history
- Early onset of menstruation or short menstrual cycles
- Heavy, painful, or prolonged periods
- Hormonal imbalances, especially unopposed estrogen
- High levels of systemic inflammation
- Immune system dysregulation
- Environmental toxin exposure (e.g., xenoestrogens from plastics, pesticides)
- Poor gut health, which can impair estrogen metabolism and immune response
Endometriosis is not just a “reproductive issue”—it’s a whole-body condition that often coexists with IBS, autoimmune disorders, anxiety, fatigue, and chronic pain syndromes.
Holistic Strategies for Managing Endometriosis
At Antigravity Wellness, we take a comprehensive, root-cause approach to endometriosis that supports the whole woman—not just her uterus.
✅ Nutrition
- Focus on an anti-inflammatory diet: leafy greens, wild-caught fish, berries, turmeric, and cruciferous vegetables
- Reduce or eliminate: gluten, dairy, alcohol, caffeine, and refined sugars
- Support estrogen clearance with fiber, cruciferous veggies, and flaxseeds
- Increase magnesium-rich foods like pumpkin seeds, spinach, and dark chocolate
✅ Movement
- Gentle, consistent activity helps reduce inflammation and improve circulation
- Include pelvic floor therapy, yoga, and low-impact strength training
✅ Stress & Mindset
- Chronic stress increases inflammation and pain sensitivity
- Incorporate breathwork, somatic release, journaling, and mindfulness practices
- Use tools like vagal nerve activation to calm the pain response
✅ Gut & Liver Support
- Optimize digestion and bowel regularity to prevent estrogen recirculation
- Consider probiotics, bitters, and liver-supporting herbs (like dandelion root or milk thistle) under provider guidance
Advanced Testing at Antigravity Wellness
Endometriosis is complex—but the more data we have, the more effective and personalized your care can be.
At Antigravity Wellness, we offer advanced functional testing, including:
- DUTCH hormone testing to evaluate estrogen, progesterone, cortisol, and detox pathways
- GI MAP testing to assess gut inflammation, infections, and microbiome balance
- Food sensitivity panels
- Thyroid and adrenal function labs
- Comprehensive metabolic and inflammatory markers
With this level of insight, we can uncover what’s driving your endometriosis—and create a clear, actionable plan.
Conventional Medical Treatments
Mainstream treatment options include:
- Hormonal birth control (to suppress estrogen)
- Progestin-based IUDs or oral medications
- GnRH agonists (like Lupron), which induce temporary menopause
- Laparoscopic surgery to remove lesions and adhesions
- NSAIDs or pain medications
While these can help with symptom control, they often come with side effects—and rarely address the root cause. Surgery can provide relief but may not prevent recurrence without holistic support.
Case Study: Meet Dana
Dana, 42, came to Antigravity Wellness with a 20-year history of painful periods, bloating, IBS symptoms, and pelvic discomfort during intimacy. She had undergone surgery for endometriosis twice, but the symptoms always came back.
Through advanced testing, we found:
- Low progesterone and poor estrogen detox pathways
- High inflammation markers
- Gut dysbiosis and leaky gut
- Poor bile flow due to a sluggish gallbladder
We created a targeted protocol that included:
- A hormone-balancing plan using bioidentical progesterone
- Gut repair with GI MAP-guided support
- A gluten- and dairy-free anti-inflammatory diet
- Liver and lymphatic support
- Nervous system regulation through breathwork and somatic tools
Within three months, Dana’s periods were manageable, her digestion normalized, and—for the first time in years—she had a full month pain-free.
Endometriosis Deserves More Than Pain Pills and Platitudes
If you’ve been told your pain is normal, if you’ve been offered birth control without an explanation, or if you’ve had surgery that didn’t fix the issue—you are not alone.
Your pain is real. Your experience is valid. And there is a better way.
Let’s uncover the root of your symptoms and build a plan that actually works—for your whole body, not just your cycle.
👉 Book your Brief Initial Consult now
👉 Explore our favorite hormone and inflammation support supplements in the Fullscript Shop
Resources and References
- Giudice LC. “Clinical practice. Endometriosis.” N Engl J Med. 2010;362(25):2389–2398. https://doi.org/10.1056/NEJMcp1000274
- Bulun SE. “Endometriosis.” N Engl J Med. 2009;360(3):268–279. https://doi.org/10.1056/NEJMra0804690
- Vercellini P, et al. “Medical treatment for rectovaginal endometriosis: what is the evidence?” Hum Reprod. 2009;24(10):2504–2514. https://doi.org/10.1093/humrep/dep275
- Impact of endometriosis on women’s health-related quality of life: A national prospective cohort study. https://www.sciencedirect.com/science/article/pii/S0378512223003596