If you’re in your late 30s, 40s, or early 50s and suddenly dealing with anxiety, poor sleep, irritability, brain fog, fatigue, or feeling like you don’t recognize yourself anymore—you’re not imagining it, and you’re not “just stressed.”
What many women are experiencing during perimenopause is not simply a hormone problem. It’s a nervous system regulation problem.
This is where polyvagal theory becomes incredibly helpful.
What is polyvagal theory?
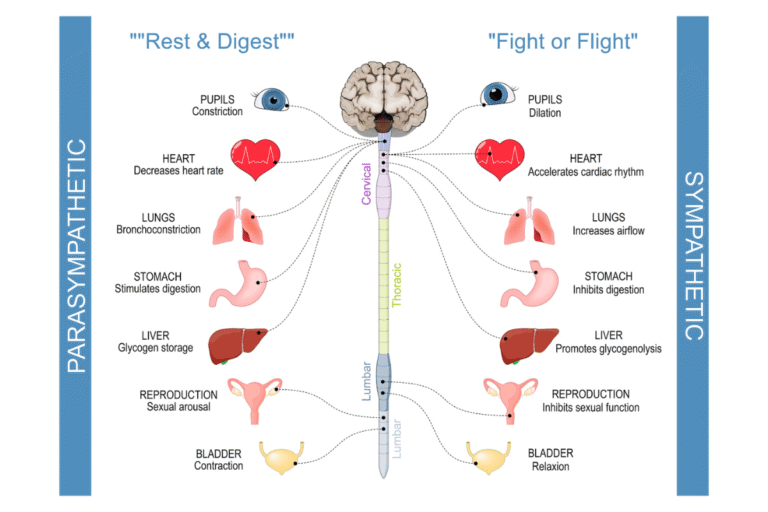
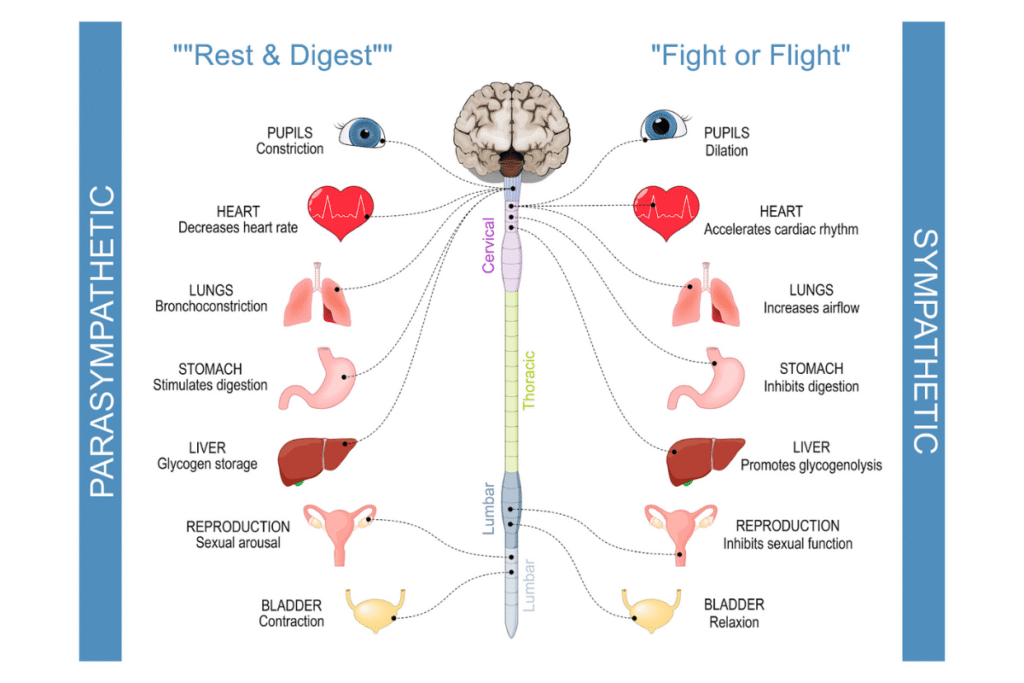
Polyvagal theory was developed by Stephen Porges and explains how our autonomic nervous system responds to safety, stress, and perceived threat.
Instead of thinking about the nervous system as just “calm” or “stressed,” polyvagal theory describes three distinct states that our bodies move through every day—often without us realizing it.
Understanding these states helps explain why so many perimenopausal symptoms feel emotional, physical, and unpredictable all at once.
The three nervous system states (in plain language)
1. Ventral Vagal: Safety, calm, and connection
This is the state where your body works best.
When you’re here:
- You feel calm but alert
- Your digestion works
- Sleep comes more easily
- Hormones communicate properly
- You feel emotionally steady and connected
This is the state where healing, repair, and hormone balance happen.
2. Sympathetic: Fight or flight
This is your stress-response system.
When activated, you may experience:
- Anxiety or panic
- Racing thoughts
- Irritability or rage
- Heart palpitations
- Hot flashes
- Insomnia
- Blood sugar crashes
This state is meant to be temporary. The problem is that many women live here chronically.
3. Dorsal Vagal: Shutdown or freeze
This is a protective “power-saving mode.”
Symptoms often include:
- Persistent fatigue
- Depression or numbness
- Low motivation
- Brain fog
- Low libido
- Feeling disconnected from yourself
This state often follows long periods of unrelenting stress.
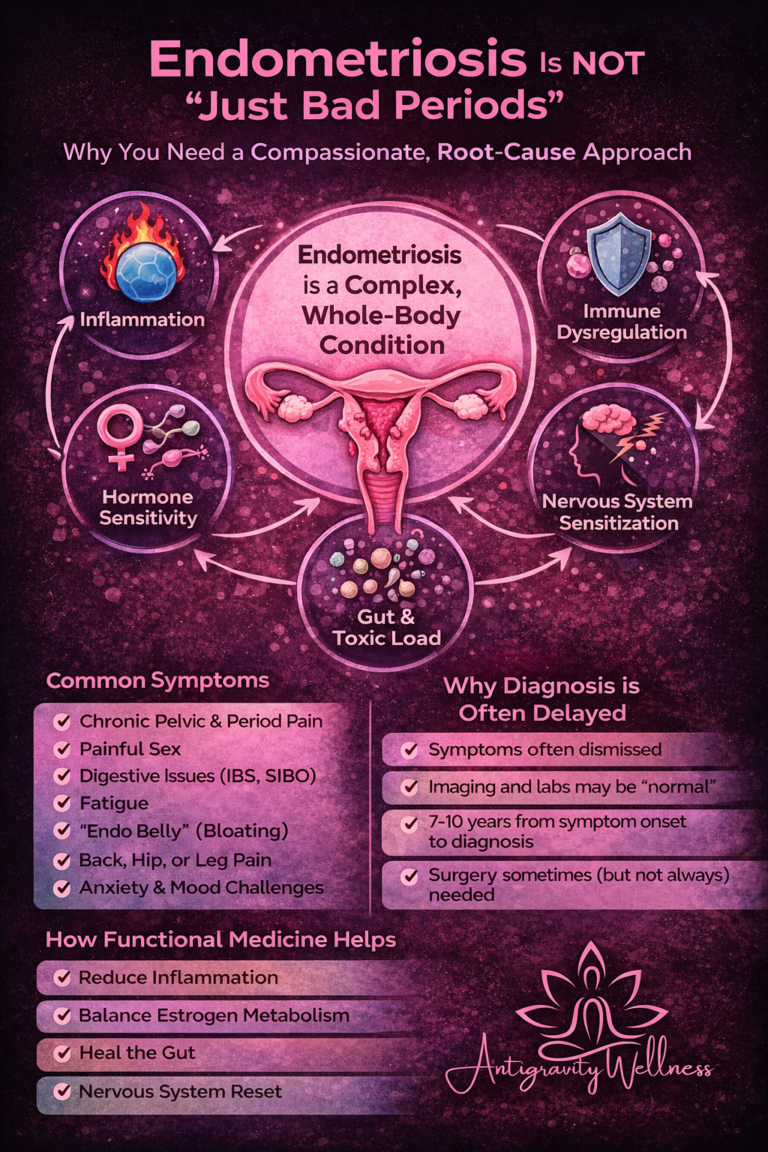
Why polyvagal theory is so relevant in perimenopause
Perimenopause is not just a hormone transition—it’s a stress amplifier.
Estrogen and progesterone regulate the nervous system
- Estrogen supports serotonin, dopamine, and vagal tone
- Progesterone has calming, GABA-supportive effects
As these hormones fluctuate:
- The nervous system becomes more reactive
- Stress tolerance drops
- The body perceives threat more easily—even when nothing is “wrong”
This is why women often say:
- “My anxiety came out of nowhere”
- “I can’t handle stress like I used to”
- “I feel on edge all the time”
- “I’m exhausted but can’t sleep”
This is not a personality flaw.
It’s biology.
Chronic stress + hormone shifts = nervous system overload
Many women entering perimenopause:
- Are high achievers
- Are caregivers
- Have spent years ignoring their own needs
- Have normalized stress and burnout
When hormones start fluctuating, the nervous system loses its buffering capacity. What used to be manageable no longer is.
The body shifts into survival mode—and stays there.
Why “just treating hormones” isn’t always enough
When the nervous system is stuck in fight/flight or shutdown:
- Cortisol remains elevated
- Thyroid conversion can suffer
- Blood sugar becomes unstable
- Estrogen detoxification worsens
- Progesterone may feel less effective
- Inflammation increases
This is why:
- Supplements stop “working”
- Hormone therapy helps but doesn’t fully resolve symptoms
- Women feel frustrated and dismissed
Hormones cannot fully regulate in a body that doesn’t feel safe.
How polyvagal-informed care supports perimenopausal women
The goal isn’t to eliminate stress (that’s impossible).
The goal is to teach the nervous system how to return to safety.
Daily nervous system regulation is non-negotiable
This isn’t self-care—it’s medical care.
Helpful practices include:
- Slow nasal breathing with longer exhales
- Walking outdoors
- Gentle strength training (not constant HIIT)
- Prayer, meditation, or guided relaxation
- Humming, singing, or gargling (vagus nerve stimulation)
- Safe, supportive connection with others
Small, consistent practices matter more than intensity.
Reframing symptoms changes physiology
When women understand that symptoms are protective responses, not failures, fear decreases.
Less fear → less sympathetic activation → improved hormone responsiveness.
Education itself becomes therapeutic.
Hormone therapy works best with nervous system support
Estrogen and progesterone can:
- Improve sleep
- Improve mood
- Support vagal tone
But they work best when paired with:
- Stress regulation
- Adequate nutrition
- Stable blood sugar
- Appropriate movement
- Rest and recovery
This is why a whole-person approach matters.
The big picture
Perimenopause is often the moment when a woman’s body finally says:
“I’ve been in survival mode for too long.”
Polyvagal theory gives language and validation to what so many women experience but struggle to explain.
This phase of life isn’t about decline.
It’s about relearning safety, restoring regulation, and rebuilding resilience.
When the nervous system feels safe again, the body becomes responsive—to hormones, nutrition, movement, and healing.
Case Study: When Hormones Weren’t the Whole Problem
(Name and identifying details changed to protect patient privacy)
“Loretta,” age 44, came to our clinic frustrated and exhausted.
She reported:
- New-onset anxiety and nighttime panic
- Poor sleep despite extreme fatigue
- Weight gain around her midsection
- Brain fog and emotional reactivity
- Worsening PMS and irregular cycles
She had already been told by a previous provider that her labs were “normal” and that she was “probably just stressed.” She was offered a low-dose antidepressant and told to try yoga.
At first glance, Loretta’s symptoms did look hormonal—and they were—but hormones were only part of the picture.
What we found
A deeper evaluation revealed:
- Clear signs of sympathetic nervous system dominance
- Long-standing high stress with no daily downregulation practices
- Blood sugar instability
- Inadequate protein intake and under-fueling
- Overuse of high-intensity exercise despite poor recovery
- Low progesterone relative to estrogen, contributing to sleep and anxiety symptoms
Her body wasn’t broken—it was stuck in survival mode.
Our approach
Instead of “throwing hormones at symptoms,” we took a polyvagal-informed, whole-body approach:
- Gentle, appropriate hormone support
- A shift from constant HIIT to strength training with recovery days
- Blood sugar stabilization through nutrition timing and adequate protein
- Daily nervous system regulation practices (breathing, walking, wind-down routines)
- Sleep support focused on circadian rhythm and safety cues
- Education around why her symptoms were protective, not pathological
The outcome
Within weeks:
- Sleep improved
- Anxiety episodes decreased dramatically
- Energy became more consistent
- Brain fog lifted
- She reported feeling “like myself again” for the first time in years
This didn’t happen because we found the perfect hormone dose.
It happened because her nervous system finally felt safe enough to respond.
How This Reflects Care at Antigravity Wellness
At Antigravity Wellness, polyvagal theory isn’t a buzzword—it’s woven into how we care for women.
We don’t believe in:
- Dismissing symptoms as “just stress”
- Treating labs without context
- Handing out hormones without addressing lifestyle, nutrition, movement, and nervous system health
Instead, we practice deeply integrated care.
That means:
- Hormones are one tool—not the only tool
- Nutrition, exercise, sleep, and stress physiology matter
- The nervous system is central to hormone balance
- Women are active participants in reclaiming their vitality
True healing happens when a woman understands her body, feels supported, and regains control over her health and her life.
Are We a Good Fit?
If you’re wondering whether this approach is right for you, the first step is clarity.
We invite you to complete our Readiness Questionnaire, which helps determine:
- Whether you’re a good fit for our model of care
- What level of support may be most appropriate
- Whether now is the right time to begin deeper work
This isn’t about convincing you to start hormones.
It’s about making sure we’re aligned in values, expectations, and goals.
👉 Take the Readiness Questionnaire to explore next steps.
Medical References
- Porges, S. W. (2011). The Polyvagal Theory: Neurophysiological Foundations of Emotions, Attachment, Communication, and Self-Regulation. W.W. Norton & Company. https://psycnet.apa.org/record/2011-04659-000
- Porges, S. W. (2021). Polyvagal Safety: Attachment, Communication, Self-Regulation. W.W. Norton & Company. https://wwnorton.com/books/9781324016274
- Gordon, J. L., et al. (2015). Estradiol variability, stress sensitivity, and mood symptoms in perimenopausal women. Archives of Women’s Mental Health, 18(5), 727–736. https://pubmed.ncbi.nlm.nih.gov/26529616/
- Brinton, R. D. (2009). Estrogen-induced plasticity from cells to circuits: predictions for cognitive function. Trends in Pharmacological Sciences, 30(4), 212–222. https://pubmed.ncbi.nlm.nih.gov/19299024/
- Claudio N Soares., et al. (2008). Reproductive hormone sensitivity and mood disorders across the female lifespan. https://pubmed.ncbi.nlm.nih.gov/18592034/
- McEwen, B. S. (2017). Neurobiological and systemic effects of chronic stress. Dialogues in Clinical Neuroscience, 19(4), 327–337. https://pubmed.ncbi.nlm.nih.gov/28856337/
- Goldstein, D. S. (2010). Adrenal responses to stress. Cellular and Molecular Neurobiology, 30(8), 1433–1440. https://pubmed.ncbi.nlm.nih.gov/21061156/
Medical DisclaimerThis article is for educational purposes only and is not intended to diagnose, treat, cure, or prevent any disease. The information provided does not replace individualized medical advice from a qualified healthcare professional. Always consult your healthcare provider before starting or changing any medical, nutritional, exercise, or hormone therapy program. Individual results may vary.