Perimenopause is a significant transition in a woman’s life, marked by hormonal shifts and physiological changes. What many women don’t realize is that perimenopause itself is an inflammatory state, creating a cascade of effects throughout the body. Combined with changes in cortisol levels, disruptions in the gut microbiome, and life’s inevitable stressors, it can feel like the perfect storm for chronic inflammation.
Understanding the signs, causes, and holistic strategies to address inflammation can help women navigate this transition with better health and vitality.
What is Inflammation?
Inflammation is the body’s natural response to injury, infection, or other stressors. It is part of the immune system’s defense mechanism and can be divided into two types:
1. Acute Inflammation
- What it is: A short-term, localized response to injury or infection (e.g., a cut or the flu).
- Symptoms: Redness, swelling, heat, pain, and loss of function.
- Purpose: To protect the body and promote healing.
2. Chronic Inflammation
- What it is: A prolonged, low-grade inflammatory response that persists over time.
- Symptoms: Often subtle, including fatigue, joint pain, digestive issues, and brain fog.
- Concern: Chronic inflammation is harmful and linked to conditions like heart disease, diabetes, autoimmune disorders, and cognitive decline.
Why Perimenopause is a Time of Increased Inflammation
1. Hormonal Shifts
- Declining estrogen levels play a key role. Estrogen has anti-inflammatory properties, so lower levels can lead to a heightened inflammatory response.
2. Changes in Cortisol Levels
- Perimenopause often brings about fluctuations in cortisol, the body’s stress hormone. Elevated cortisol can fuel inflammation, particularly when combined with ongoing stress.
3. Gut Microbiome Disruption
- Estrogen influences the gut microbiome. As levels drop, the balance of good and bad bacteria can shift, contributing to systemic inflammation and conditions like leaky gut.
4. Lifestyle Factors
- Stress, poor sleep, lack of exercise, and diets high in processed foods all exacerbate inflammation.
- The cumulative effect of life stressors during this transitional phase compounds the problem.
Signs and Symptoms of Chronic Inflammation
Recognizing the symptoms of inflammation is crucial for addressing it early:
- Fatigue or low energy levels.
- Persistent joint or muscle pain.
- Brain fog or difficulty concentrating.
- Digestive issues like bloating or irregular bowel movements.
- Weight gain, particularly around the midsection.
- Skin issues such as rashes or acne.
- Mood changes, including anxiety or depression.
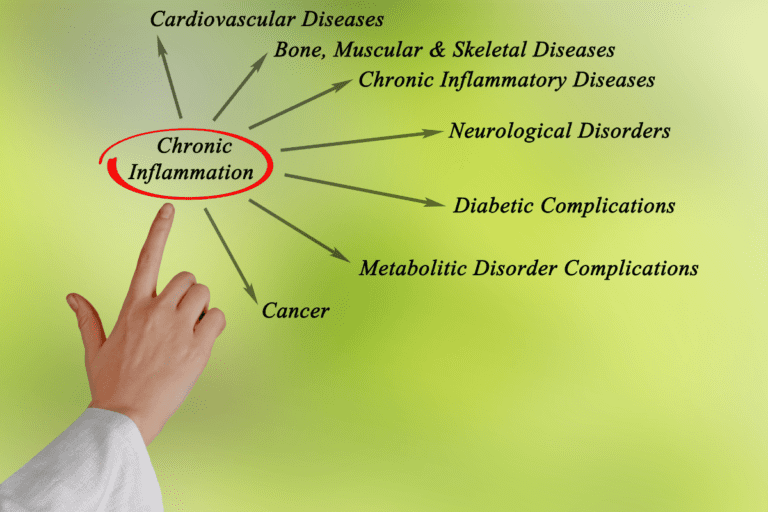
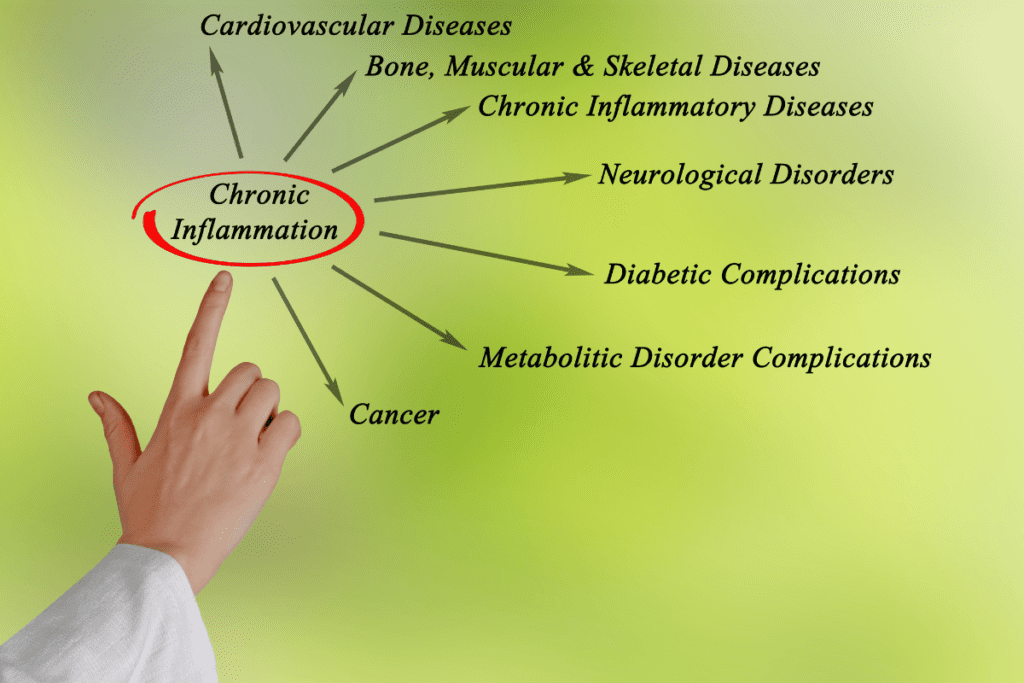
Why Chronic Inflammation is a Concern
Unlike acute inflammation, which helps the body heal, chronic inflammation quietly damages tissues and organs over time, leading to:
- Cardiovascular Disease: Inflammation contributes to plaque buildup in arteries.
- Metabolic Disorders: Insulin resistance and weight gain are exacerbated by inflammation.
- Autoimmune Disorders: Chronic inflammation increases the risk of autoimmune conditions.
- Cognitive Decline: Inflammation in the brain is linked to Alzheimer’s and other neurodegenerative diseases.
- Bone Loss: Systemic inflammation speeds up bone resorption, increasing the risk of osteoporosis.
Holistic Strategies to Address Inflammation in Perimenopause
1. Dietary Modifications
- Anti-Inflammatory Diet: Focus on whole, nutrient-dense foods like leafy greens, berries, fatty fish, nuts, and seeds.
- Avoid Inflammatory Foods: Limit sugar, processed foods, alcohol, and trans fats.
- Omega-3 Fatty Acids: Found in salmon, walnuts, and flaxseeds, these help reduce inflammation.
- Spices: Turmeric, ginger, and cinnamon have natural anti-inflammatory properties.
2. Exercise
- Regular movement reduces inflammation and supports hormonal balance.
- Include a mix of strength training, cardio, and yoga or stretching for optimal results.
3. Stress Management
- Practices like meditation, deep breathing, and journaling can lower cortisol levels.
- Adequate sleep is also essential; aim for 7–9 hours per night.
4. Herbal and Nutritional Supplements
- Curcumin: The active ingredient in turmeric, known for its anti-inflammatory properties.
- Magnesium: Helps reduce stress and inflammation.
- Probiotics: Support gut health and reduce systemic inflammation.
- Vitamin D: Crucial for immune regulation and reducing inflammation.
5. Testing and Functional Medicine
At Antigravity Wellness, we use functional labs to identify the root causes of inflammation. These may include:
- Hormone Panels: Assess estrogen, progesterone, testosterone, and cortisol levels.
- Gut Health Testing: Identify imbalances in the gut microbiome or leaky gut.
- Inflammatory Markers: C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) measure systemic inflammation.
- Nutritional Deficiencies: Test for deficiencies in vitamin D, magnesium, omega-3s, and other anti-inflammatory nutrients.
Further Reading and Resources
- The Inflammation Spectrum by Dr. Will Cole
- Hormone Repair Manual by Lara Briden
- Research Articles:
Addressing Inflammation with Antigravity Wellness
At Antigravity Wellness, we understand the intricate connections between inflammation, hormonal shifts, and overall health during perimenopause. Using a holistic approach, we target the root causes of inflammation with:
- Personalized dietary and lifestyle plans.
- Functional testing to pinpoint areas of concern.
- Nutritional and herbal supplementation tailored to your needs.
If you’re struggling with inflammation and its effects, we can help you reverse the damage and restore balance. Schedule a brief initial consult today to take the first step toward feeling and functioning better.